Malformasi arteri-vena: Perbedaan antara revisi
Tidak ada ringkasan suntingan |
Tidak ada ringkasan suntingan |
||
| Baris 13: | Baris 13: | ||
* Sensasi abnormal (kebas, kesemutan, atau nyeri tiba-tiba); |
* Sensasi abnormal (kebas, kesemutan, atau nyeri tiba-tiba); |
||
* Gangguan daya ingat dan pikir, seperti pusing, demensia, atau halusinasi.<ref name="NINDS">{{NINDS|Arteriovenous-Malformation|Arteriovenous Malformation Information Page}}</ref> |
* Gangguan daya ingat dan pikir, seperti pusing, demensia, atau halusinasi.<ref name="NINDS">{{NINDS|Arteriovenous-Malformation|Arteriovenous Malformation Information Page}}</ref> |
||
== Pathophysiology == |
|||
Arteries and veins are part of the [[Circulatory system|vascular system]]. Arteries carry blood away from the heart to the lungs or the rest of the body, where the blood passes through capillaries, and veins return the blood to the heart. An AVM interferes with this process by forming a direct connection of the arteries and veins. AVMs can cause intense pain and lead to serious medical problems. Although AVMs are often associated with the brain and spinal cord, they can develop in any part of the body. |
|||
Normally, the arteries in the vascular system carry oxygen-rich blood, except in the case of the pulmonary artery. Structurally, arteries divide and sub-divide repeatedly, eventually forming a sponge-like [[capillary bed]]. Blood moves through the [[Capillary|capillaries]], giving up oxygen and taking up waste products, including {{chem|CO|2|link=Carbon dioxide}}, from the surrounding cells. Capillaries in turn successively join together to form veins that carry blood away. The heart acts to pump blood through arteries and uptake the venous blood. |
|||
As an AVM lacks the dampening effect of capillaries on the blood flow, the AVM can get progressively larger over time as the amount of blood flowing through it increases, forcing the heart to work harder to keep up with the extra blood flow. It also causes the surrounding area to be deprived of the functions of the capillaries—removal of {{CO2}} and delivery of nutrients to the cells. The resulting tangle of blood vessels, often called a ''nidus'' (Latin for "nest"), has no capillaries. It can be extremely fragile and prone to bleeding because of the abnormally direct connections between high-pressure arteries and low-pressure veins. The resultant sign, audible via [[stethoscope]], is a rhythmic, whooshing sound caused by excessively rapid blood flow through the arteries and veins. It has been given the term "bruit", French for noise. On some occasions, a patient with a brain AVM may become aware of the noise, which can compromise hearing and interfere with sleep in addition to causing psychological distress. |
|||
== Diagnosis == |
|||
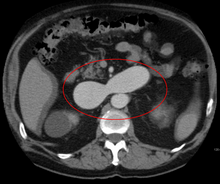
[[Berkas:PleftkidneyAVM1.png|jmpl|An arterial venous malformation of the left kidney and a simple cyst of the right kidney]] |
|||
[[Berkas:PleftkidneyAVM2.png|jmpl|An arterial venous malformation of the left kidney leading to aneurysmal dilatation of the left renal vein and inferior vena cava]] |
|||
AVMs are diagnosed primarily by the following [[Medical imaging|imaging methods]]: |
|||
* [[Computerized tomography]] (CT) scan is a noninvasive X-ray to view the anatomical structures within the brain to detect blood in or around the brain. A newer technology called [[CT angiography]] involves the injection of contrast into the blood stream to view the arteries of the brain. This type of test provides the best pictures of blood vessels through angiography and soft tissues through CT. |
|||
* [[Magnetic resonance imaging]] (MRI) scan is a noninvasive test, which uses a magnetic field and radio-frequency waves to give a detailed view of the soft tissues of the brain. |
|||
* [[Magnetic resonance angiography]] (MRA) – scans created using magnetic resonance imaging to specifically image the blood vessels and structures of the brain. A magnetic resonance angiogram can be an invasive procedure, involving the introduction of contrast dyes (e.g., gadolinium MR contrast agents) into the vasculature of a patient using a catheter inserted into an artery and passed through the blood vessels to the brain. Once the catheter is in place, the contrast dye is injected into the bloodstream and the MR images are taken. Additionally or alternatively, flow-dependent or other contrast-free magnetic resonance imaging techniques can be used to determine the location and other properties of the vasculature. |
|||
AVMs can occur in various parts of the body: |
|||
* [[Human brain|brain]] ([[Cerebral arteriovenous malformation|cerebral AV malformation]]) |
|||
* [[spleen]]<ref name="pmid17145440">{{cite journal|last1=Agrawal|first1=Aditya|last2=Whitehouse|first2=Richard|last3=Johnson|first3=Robert W.|last4=Augustine|first4=Titus|year=2006|title=Giant splenic artery aneurysm associated with arteriovenous malformation|journal=Journal of Vascular Surgery|volume=44|issue=6|pages=1345–9|doi=10.1016/j.jvs.2006.06.049|pmid=17145440}}</ref> |
|||
* [[Human lung|lung]]<ref name="pmid18294908">{{cite journal|last1=Chowdhury|first1=Ujjwal K.|last2=Kothari|first2=Shyam S.|last3=Bishnoi|first3=Arvind K.|last4=Gupta|first4=Ruchika|last5=Mittal|first5=Chander M.|last6=Reddy|first6=Srikrishna|year=2009|title=Successful Lobectomy for Pulmonary Arteriovenous Malformation Causing Recurrent Massive Haemoptysis|journal=Heart, Lung and Circulation|volume=18|issue=2|pages=135–9|doi=10.1016/j.hlc.2007.11.142|pmid=18294908}}</ref><ref>{{Cite journal|last=Cusumano|first=Lucas R.|last2=Duckwiler|first2=Gary R.|last3=Roberts|first3=Dustin G.|last4=McWilliams|first4=Justin P.|date=2019-08-30|title=Treatment of Recurrent Pulmonary Arteriovenous Malformations: Comparison of Proximal Versus Distal Embolization Technique|journal=Cardiovascular and Interventional Radiology|doi=10.1007/s00270-019-02328-0|issn=1432-086X|pmid=31471718}}</ref> |
|||
* [[kidney]]<ref name="pmid16794894">{{cite journal|last1=Barley|first1=Fay L.|last2=Kessel|first2=David|last3=Nicholson|first3=Tony|last4=Robertson|first4=Iain|year=2006|title=Selective Embolization of Large Symptomatic Iatrogenic Renal Transplant Arteriovenous Fistula|journal=CardioVascular and Interventional Radiology|volume=29|issue=6|pages=1084–7|doi=10.1007/s00270-005-0265-z|pmid=16794894}}</ref> |
|||
* [[spinal cord]]<ref name="pmid15730991">{{cite journal|last1=Kishi|first1=K|last2=Shirai|first2=S|last3=Sonomura|first3=T|last4=Sato|first4=M|year=2005|title=Selective conformal radiotherapy for arteriovenous malformation involving the spinal cord|journal=The British Journal of Radiology|volume=78|issue=927|pages=252–4|doi=10.1259/bjr/50653404|pmid=15730991}}</ref> |
|||
* [[liver]]<ref name="pmid7650340">{{cite journal|last1=Bauer|first1=Tilman|last2=Britton|first2=Peter|last3=Lomas|first3=David|last4=Wight|first4=Derek G.D.|last5=Friend|first5=Peter J.|last6=Alexander|first6=Graeme J.M.|year=1995|title=Liver transplantation for hepatic arteriovenous malformation in hereditary haemorrhagic telangiectasia|journal=Journal of Hepatology|volume=22|issue=5|pages=586–90|doi=10.1016/0168-8278(95)80455-2|pmid=7650340}}</ref> |
|||
* [[intercostal space]]<ref name="pmid17056881">{{cite journal|last1=Rivera|first1=Peter P.|last2=Kole|first2=Max K.|last3=Pelz|first3=David M.|last4=Gulka|first4=Irene B.|last5=McKenzie|first5=F. Neil|last6=Lownie|first6=Stephen P.|year=2006|title=Congenital Intercostal Arteriovenous Malformation|journal=American Journal of Roentgenology|volume=187|issue=5|pages=W503–6|doi=10.2214/AJR.05.0367|pmid=17056881}}</ref> |
|||
* [[Iris (anatomy)|iris]]<ref name="pmid16534057">{{cite journal|last1=Shields|first1=Jerry A.|last2=Streicher|first2=Theodor F. E.|last3=Spirkova|first3=Jane H. J.|last4=Stubna|first4=Michal|last5=Shields|first5=Carol L.|year=2006|title=Arteriovenous Malformation of the Iris in 14 Cases|journal=Archives of Ophthalmology|volume=124|issue=3|pages=370–5|doi=10.1001/archopht.124.3.370|pmid=16534057}}</ref> |
|||
* [[spermatic cord]]<ref name="pmid17939869">{{cite journal|last1=Sountoulides|first1=Petros|last2=Bantis|first2=Athanasios|last3=Asouhidou|first3=Irene|last4=Aggelonidou|first4=Hellen|year=2007|title=Arteriovenous malformation of the spermatic cord as the cause of acute scrotal pain: a case report|journal=Journal of Medical Case Reports|volume=1|issue=|pages=110|doi=10.1186/1752-1947-1-110|pmc=2194703|pmid=17939869}}</ref> |
|||
* extremities – arm, shoulder, etc. |
|||
AVMs may occur in isolation or as a part of another disease (for example, [[Von Hippel-Lindau disease]] or [[hereditary hemorrhagic telangiectasia]]). |
|||
AVMs have been shown to be associated with [[aortic stenosis]].<ref>{{cite journal|last1=Batur|first1=Pelin|last2=Stewart|first2=William J.|last3=Isaacson|first3=J. Harry|year=2003|title=Increased Prevalence of Aortic Stenosis in Patients With Arteriovenous Malformations of the Gastrointestinal Tract in Heyde Syndrome|journal=Archives of Internal Medicine|volume=163|issue=15|pages=1821–4|doi=10.1001/archinte.163.15.1821|pmid=12912718}}</ref> |
|||
Bleeding from an AVM can be relatively mild or devastating. It can cause severe and less often fatal [[Stroke|strokes]]. If a cerebral AVM is detected before a stroke occurs, usually the arteries feeding blood into the nidus can be closed off to avert the danger. However, interventional therapy may also be relatively risky.<!-- The cerebral arteriovenous malformation article states that benefits of such intervention have not been proven to outweigh risk; ongoing international study mentioned below. --> |
|||
== Referensi == |
== Referensi == |
||
Revisi per 1 April 2020 16.24
Halaman ini sedang dipersiapkan dan dikembangkan sehingga mungkin terjadi perubahan besar. Anda dapat membantu dalam penyuntingan halaman ini. Halaman ini terakhir disunting oleh Ardzun (Kontrib • Log) 1504 hari 219 menit lalu. Jika Anda melihat halaman ini tidak disunting dalam beberapa hari, mohon hapus templat ini. |
| Malformasi arteri vena | |
|---|---|
 | |
| Gambaran jaringan malformasi arteri vena di otak. | |
| Informasi umum | |
| Nama lain | AVM |
| Spesialisasi | Bedah saraf |
Malformasi arteri-vena (MAV) (Inggris: Arteriovenous Malformation (AVM)) adalah kondisi abnormal dari arteri dan vena yang diperantarai sistem kapiler. Anomali pembuluh darah ini secara luas diketahui terjadi pada sistem saraf pusat. Walau begitu, dapat terjadi di banyak tempat dalam tubuh manusia. Malformasi arteri-vena dapat terjadi tanpa gejala hingga memunculkan rasa nyeri yang hebat, perdarahan, atau memicu masalah medis berat. Malformasi arteri vena biasanya kongenital atau bawaan lahir.
Tanda dan gejala
Gejala dari MAV dapat beragam tergantung lokasi terjadinya malformasi. Sebagian besar penderita MAV tidak memiliki gejala apapun. Bahkan, MAV lebih sering diketahui ketika dilakukan tindakan otopsi atau saat dilakukan pengobatan yang tidak terkait dengan gangguan yang ada. Pada kasus yang jarang, pelebaran arau perdarahan akibat MAV di otak dapat menyebabkan epilepsi, defisit neurologis, atau nyeri.[1]
Gejala yang paling sering muncul pada MAV otak antara lain sakit kepala dan kejang epilepsi. Gejala yang muncul dapat menunjukkan area terjadinya malformasi. Gejala-gejala yang dapat muncul antara lain :
- Kesulitan koordinasi anggota gerak;
- Vertigo atau rasa pusing berputar;
- Sulit berbicara (disartria) dan komunikasi, seperti afasia
- Sulit untuk aktivitas harian, seperti apraksia
- Sensasi abnormal (kebas, kesemutan, atau nyeri tiba-tiba);
- Gangguan daya ingat dan pikir, seperti pusing, demensia, atau halusinasi.[2]
Pathophysiology
Arteries and veins are part of the vascular system. Arteries carry blood away from the heart to the lungs or the rest of the body, where the blood passes through capillaries, and veins return the blood to the heart. An AVM interferes with this process by forming a direct connection of the arteries and veins. AVMs can cause intense pain and lead to serious medical problems. Although AVMs are often associated with the brain and spinal cord, they can develop in any part of the body.
Normally, the arteries in the vascular system carry oxygen-rich blood, except in the case of the pulmonary artery. Structurally, arteries divide and sub-divide repeatedly, eventually forming a sponge-like capillary bed. Blood moves through the capillaries, giving up oxygen and taking up waste products, including CO2, from the surrounding cells. Capillaries in turn successively join together to form veins that carry blood away. The heart acts to pump blood through arteries and uptake the venous blood.
As an AVM lacks the dampening effect of capillaries on the blood flow, the AVM can get progressively larger over time as the amount of blood flowing through it increases, forcing the heart to work harder to keep up with the extra blood flow. It also causes the surrounding area to be deprived of the functions of the capillaries—removal of CO2 and delivery of nutrients to the cells. The resulting tangle of blood vessels, often called a nidus (Latin for "nest"), has no capillaries. It can be extremely fragile and prone to bleeding because of the abnormally direct connections between high-pressure arteries and low-pressure veins. The resultant sign, audible via stethoscope, is a rhythmic, whooshing sound caused by excessively rapid blood flow through the arteries and veins. It has been given the term "bruit", French for noise. On some occasions, a patient with a brain AVM may become aware of the noise, which can compromise hearing and interfere with sleep in addition to causing psychological distress.
Diagnosis

AVMs are diagnosed primarily by the following imaging methods:
- Computerized tomography (CT) scan is a noninvasive X-ray to view the anatomical structures within the brain to detect blood in or around the brain. A newer technology called CT angiography involves the injection of contrast into the blood stream to view the arteries of the brain. This type of test provides the best pictures of blood vessels through angiography and soft tissues through CT.
- Magnetic resonance imaging (MRI) scan is a noninvasive test, which uses a magnetic field and radio-frequency waves to give a detailed view of the soft tissues of the brain.
- Magnetic resonance angiography (MRA) – scans created using magnetic resonance imaging to specifically image the blood vessels and structures of the brain. A magnetic resonance angiogram can be an invasive procedure, involving the introduction of contrast dyes (e.g., gadolinium MR contrast agents) into the vasculature of a patient using a catheter inserted into an artery and passed through the blood vessels to the brain. Once the catheter is in place, the contrast dye is injected into the bloodstream and the MR images are taken. Additionally or alternatively, flow-dependent or other contrast-free magnetic resonance imaging techniques can be used to determine the location and other properties of the vasculature.
AVMs can occur in various parts of the body:
- brain (cerebral AV malformation)
- spleen[3]
- lung[4][5]
- kidney[6]
- spinal cord[7]
- liver[8]
- intercostal space[9]
- iris[10]
- spermatic cord[11]
- extremities – arm, shoulder, etc.
AVMs may occur in isolation or as a part of another disease (for example, Von Hippel-Lindau disease or hereditary hemorrhagic telangiectasia).
AVMs have been shown to be associated with aortic stenosis.[12]
Bleeding from an AVM can be relatively mild or devastating. It can cause severe and less often fatal strokes. If a cerebral AVM is detected before a stroke occurs, usually the arteries feeding blood into the nidus can be closed off to avert the danger. However, interventional therapy may also be relatively risky.
Referensi
- ^ "National Institute of Neurological Disorders and Stroke". nih.gov. Diakses tanggal 17 March 2018.
- ^ Arteriovenous Malformation Information Page pada NINDS
- ^ Agrawal, Aditya; Whitehouse, Richard; Johnson, Robert W.; Augustine, Titus (2006). "Giant splenic artery aneurysm associated with arteriovenous malformation". Journal of Vascular Surgery. 44 (6): 1345–9. doi:10.1016/j.jvs.2006.06.049. PMID 17145440.
- ^ Chowdhury, Ujjwal K.; Kothari, Shyam S.; Bishnoi, Arvind K.; Gupta, Ruchika; Mittal, Chander M.; Reddy, Srikrishna (2009). "Successful Lobectomy for Pulmonary Arteriovenous Malformation Causing Recurrent Massive Haemoptysis". Heart, Lung and Circulation. 18 (2): 135–9. doi:10.1016/j.hlc.2007.11.142. PMID 18294908.
- ^ Cusumano, Lucas R.; Duckwiler, Gary R.; Roberts, Dustin G.; McWilliams, Justin P. (2019-08-30). "Treatment of Recurrent Pulmonary Arteriovenous Malformations: Comparison of Proximal Versus Distal Embolization Technique". Cardiovascular and Interventional Radiology. doi:10.1007/s00270-019-02328-0. ISSN 1432-086X. PMID 31471718.
- ^ Barley, Fay L.; Kessel, David; Nicholson, Tony; Robertson, Iain (2006). "Selective Embolization of Large Symptomatic Iatrogenic Renal Transplant Arteriovenous Fistula". CardioVascular and Interventional Radiology. 29 (6): 1084–7. doi:10.1007/s00270-005-0265-z. PMID 16794894.
- ^ Kishi, K; Shirai, S; Sonomura, T; Sato, M (2005). "Selective conformal radiotherapy for arteriovenous malformation involving the spinal cord". The British Journal of Radiology. 78 (927): 252–4. doi:10.1259/bjr/50653404. PMID 15730991.
- ^ Bauer, Tilman; Britton, Peter; Lomas, David; Wight, Derek G.D.; Friend, Peter J.; Alexander, Graeme J.M. (1995). "Liver transplantation for hepatic arteriovenous malformation in hereditary haemorrhagic telangiectasia". Journal of Hepatology. 22 (5): 586–90. doi:10.1016/0168-8278(95)80455-2. PMID 7650340.
- ^ Rivera, Peter P.; Kole, Max K.; Pelz, David M.; Gulka, Irene B.; McKenzie, F. Neil; Lownie, Stephen P. (2006). "Congenital Intercostal Arteriovenous Malformation". American Journal of Roentgenology. 187 (5): W503–6. doi:10.2214/AJR.05.0367. PMID 17056881.
- ^ Shields, Jerry A.; Streicher, Theodor F. E.; Spirkova, Jane H. J.; Stubna, Michal; Shields, Carol L. (2006). "Arteriovenous Malformation of the Iris in 14 Cases". Archives of Ophthalmology. 124 (3): 370–5. doi:10.1001/archopht.124.3.370. PMID 16534057.
- ^ Sountoulides, Petros; Bantis, Athanasios; Asouhidou, Irene; Aggelonidou, Hellen (2007). "Arteriovenous malformation of the spermatic cord as the cause of acute scrotal pain: a case report". Journal of Medical Case Reports. 1: 110. doi:10.1186/1752-1947-1-110. PMC 2194703
 . PMID 17939869.
. PMID 17939869.
- ^ Batur, Pelin; Stewart, William J.; Isaacson, J. Harry (2003). "Increased Prevalence of Aortic Stenosis in Patients With Arteriovenous Malformations of the Gastrointestinal Tract in Heyde Syndrome". Archives of Internal Medicine. 163 (15): 1821–4. doi:10.1001/archinte.163.15.1821. PMID 12912718.
